CBT
Cognitive Behavior Therapy for Neuropsychiatric Disorders
Cognitive Behavior Therapy (CBT) can be helpful for patients with functional neurological disorders, persistent post-concussive symptoms, traumatic brain injury, chronic pain, PTSD, and coping with neurological illness. It is influenced by learning theory, social learning theory, and cognitive neuroscience.
Principles of Cognitive Behavior Therapy
CBT typically consists of sessions 1-2 times per week. Short-term treatment may be from 2-6 months. Long-term treatment can last several years. Short-term treatment tends to have very specific goals while long-term treatment tends to focus on dealing with entrenched patterns of thinking, feeling and being.
In treatment, the therapist focuses on the relationship between thoughts, feelings, actions, and events. You learn to become aware of how your thoughts, feelings, and actions affect one another and identify triggers for specific thoughts and feelings. You become aware of factors that reinforce unhelpful behaviors and challenge forms of avoidance or safety behaviors - actions that you do to protect yourself but actually ultimately make things worse for you. The therapist may use exposure or desensitization techniques to help you become more comfortable with situations you have been avoiding or otherwise dread.
The therapist also helps you challenge automatic negative thoughts by identifying the thinking traps that underlie them (e.g. all-or-nothing thinking, magnifying negatives and minimizing positives, personalizing things, jumping to conclusions, overgeneralizing, emotional reasoning, etc). The therapist might challenge you to assess the underlying assumptions behind these bothersome thoughts and identify the rules for living you've developed based on early experiences.
Main principles of the cognitive-behavioral approach are:
Behaviors are learned and can be unlearned.
Our behavior is conditioned by pleasure, pain, and social learning.
Our attitudes, beliefs, and perceptions shape our emotional response to events.
Information processing errors underlie emotional disorders.
The way we experience the world is shaped by rules for living we adopt based on early experiences
CBT for Functional Neurological Disorders
A modified CBT approach to therapy can be very helpful for some people with FND. Therapy will help you to understand verbalize and express emotions, regulate powerful emotions, assert for your emotional needs, and identify the relationship between thoughts, feelings, FND symptoms, and events. The diagnosis of FND may be confusing. You may worry you have been misdiagnosed. You may be concerned you have a serious or life-threatening illness. You may feel very alone. You may feel broken, damaged, weak, fear you are going crazy, or that the condition is "all in your head" even though nothing could be further from the truth.
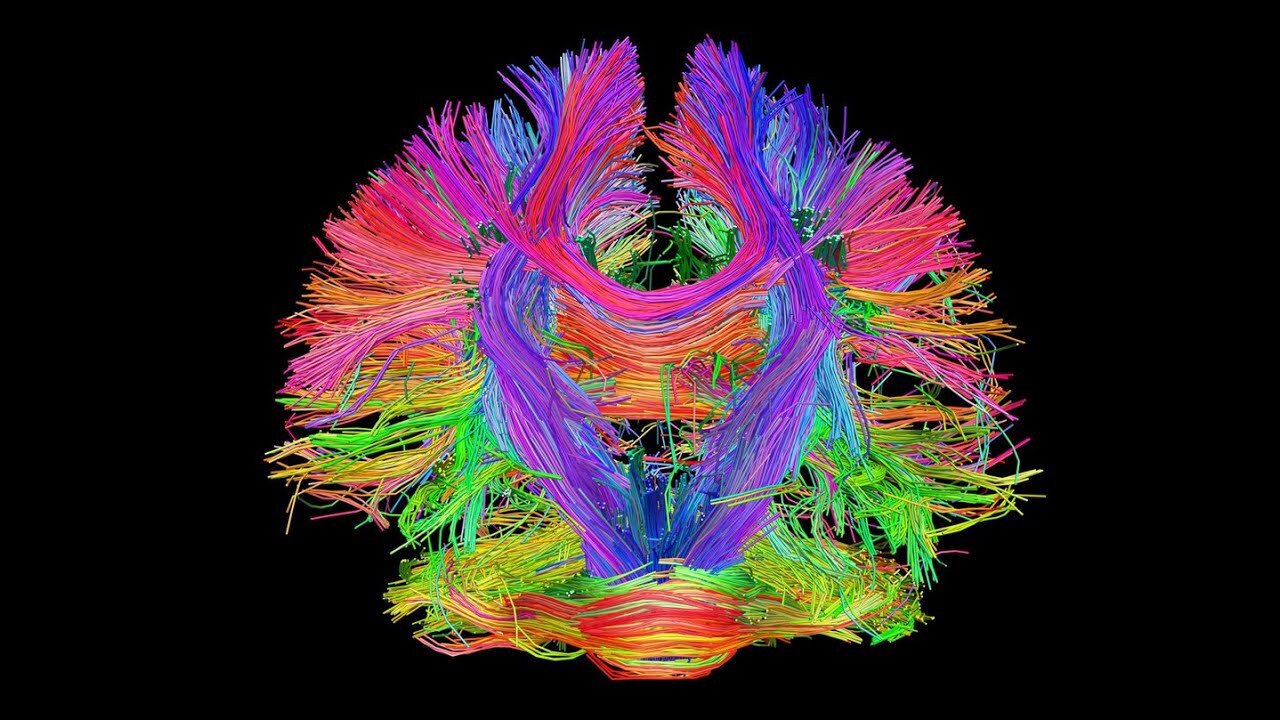
Many people with FND learned it was "better not to feel" and developed special strategies to disconnect from their emotions growing up. You may have also learned to put other people's needs above your own. You may have difficulty being able to express powerful emotions such as anger and rage. You may have difficulty advocating for your own emotional needs even if you are assertive in other ways. Failure to express powerful emotions means the brain never lets go of those emotions, and the emotional centers in the brain like the amygdala "overheat" and short circuit other brain functions leading to FND symptoms. Some studies suggest CBT informed therapy may enhance the connections involved between the emotional and language circuits in the brain.
CBT techniques can help people with FND become more aware of their automatic thoughts, thinking traps, and core beliefs. Often there are triggers that bring on or exacerbate symptoms that you can become aware of by keeping symptom and thought records. Using CBT techniques, you can identify triggers and warning signs, as well as bothersome thoughts connected to your FND symptoms. This helps retrain your brain, which rewires and no longer sends signals from the emotional brain to other brain areas incorrectly.
Over time, this can lead to a reduction in frequency or severity of symptoms or event complete elimination. In addition, CBT can help you challenge inaccurate beliefs about what it means to have this diagnosis that may cause distress or make it harder to accept what is happening. You will identify factors that might trigger or reinforce symptoms, and become aware of emotions. Often techniques based on mindfulness and DBT (e.g. distress tolerance, interpersonal effectiveness) and ACT (e.g. observing thoughts, being present, values) are incorporated into treatment.
CBT for Traumatic Brain Injury
Traumatic Brain Injury can impact physical and psychological health, change your personality, alter your identity and sense of self, and strain relationships. Following a TBI you may grieve for the loss of your health and former sense of self. Everything may seem much harder. You may fear you have lost yourself and that things will never get better. You may worry about losing people closest to you. The circumstances that led to your TBI may be traumatic and continue to haunt you.
CBT can help you to set goals, develop skills to help you work around difficulties you have, and identify triggers for symptoms, develop self-compassion, look at inaccurate thoughts you've developed about yourself and the thinking traps that underlie them, and banish avoidance and self-defeating behaviors.
This therapy is not usually appropriate for people who have severe cognitive deficits from TBI. However many other people can benefit. A neuropsychiatrist has the benefit of understanding not only the psychological effects of TBI but also how the brain injury itself can impact emotions, thoughts and behaviors. Dr. Datta is also experienced working with patients who do have some degree of cognitive impairment or language problems and modify therapy appropriately. However in the most severe cases, this kind of therapy may not be helpful other than behavior modification.
CBT for Coping with Neurological Illness
Most people coping with serious neurological illnesses can benefit from supportive psychotherapy interventions. This includes having a safe place to talk about the emotional impact of your diagnosis and what it means to you. Being heard, and receiving empathic validation, reflection, and thoughtful questioning can be very powerful and healing for some. A good therapist will also provide context for your experiences and emotions and be able to normalize and communicate the universal nature of some of those feelings so you feel less alone.
For some people, the impact of neurological illness is more hard hitting. You may feel very vulnerable, defective, worry your partner will leave you, or experience an existential conflict. You may be overwhelmed by feelings of grief, sadness, worry, panic, shame, anger, or aloneness. Some of this may be related to the traumatic nature of some symptoms (e.g. seizures) or medical procedures. Some of this may be related to how other people have responded to you. And some of it will be related to how you've processed your illness based on your own past experiences. In these cases, CBT can help you identify negative thoughts that make you feel bad, the thinking traps behind them, the underlying beliefs that are being activated, and challenge problematic avoidant and safety behaviors. You can also develop skills with progressive muscle relaxation, mindfulness, and self-compassion.
CBT for PTSD
The two main CBT approaches to posttraumatic stress disorder are Cognitive Processing Therapy (CPT), and Prolonged Exposure (PE). Dr. Datta offers CPT. The Cognitive-Behavioral Model of PTSD is based on the theory that the symptoms of PTSD are a normal initial response to a traumatic event. When something awful happens it is normal to keep thinking about it, be shaken up, hyper-vigilant, suspicious, depressed, have difficulty sleeping, and have nightmares. But typically this response will fade over time. When it doesn't, this is because of avoidant behaviors that prevent us from processing our emotions about what happened or because of stuck points we develop about the event[s] that generate powerful emotions that prevent us from healing.
Both CPT and PE involve creating a written account of the traumatic event and allowing you to feel all of the feelings that go along with it and create a more coherent narrative of what happened drawing on all of your senses (sights, sounds, smells, sensations, etc). However, CPT mainly focuses on identifying those thoughts that bring up powerful feelings that prevent you from moving on (stuck points).
Some people can't remember exactly what happened, for example due to a brain injury, or losing consciousness, or being intoxicated at the time (or even due to the psychological trauma response). In these cases, CPT-C (Cognitive Processing Therapy- Cognitive only) which does not include the written trauma account and focuses more on challenging those stuck points may be as effective.
Individuals who are actively suicidal, experiencing mania or psychosis, abusing substances, or engaging in self-destructive behaviors may need further stabilization before this therapy or else need to receive care in a residential setting. Individuals with more complex protracted trauma may benefit less from this kind of treatment and need more long term treatment. Those with severe cognitive impairment may not be able to benefit from this treatment.